Many patients do not know how to understand that you have osteochondrosis, but at the same time are happy to make such a diagnosis. Meanwhile, the causes of back, lower back or neck pain can be many. These can be curvature of the spine, disruption of internal organs, tumors, infections, instability of the position of the vertebral bodies, etc. Sh. Therefore, you should not ask a self-diagnosis. In case of pain, seek medical help.
There is no reliable algorithm for how to diagnose osteochondrosis without special examinations. But there are certain clinical signs that make it possible to suspect this disease. We will talk about them in the material in the center of your attention. In the meantime, I recommend that you familiarize yourself with the mechanism of development of osteochondrosis.
Degenerative dystrophic disease of the cartilage tissue of the intervertebral discs - so scientifically called osteochondrosis. Its development causes dorsopathy, which is complicated by dorsalgia, sciatica, sciatica, sciatica, lumbago and other syndromes associated with damage to various tissues.
Osteochondrosis is the result of maintaining a wrong human lifestyle. Contributing factors are:
- Excess body weight - each kilogram creates additional wear and mechanical load on the cartilaginous tissue of the intervertebral disc;
- A lifeless lifestyle without regular exercise on the spinal cord;
- Intake of large amounts of carbohydrates, refined foods;
- Wearing tight, uncomfortable clothing and shoes;
- Wrong posture, the habit of leaning, leaning, leaning in one direction or another on the body;
- Improper foot placement in the form of flat feet or eyelids;
- Curvature of the spinal column;
- Sedentary work or hard physical labor;
- Smoking and drinking alcohol;
- Insufficient consumption of clean drinking water during the day.
All these factors slow down the blood microcirculation in the capillary network to the thickness of the muscle tissue. It turns out it fails to fully diffuse exchange with the cartilaginous tissues of the intervertebral discs. They do not have their own circulatory system. Thus begins the mechanism of destruction of the fiber ring surface (this is the outer shell of the disc). It forms a deposit of calcium salts. They prevent fluid intake from the outside. Therefore, the fibrous ring begins to remove fluid from the pulpus nucleus inside it. This gelatin body is responsible for maintaining the normal height and shape of the intervertebral disc. Therefore with loss of fluid the nucleus pulposus loses the ability to maintain the height of the disc. The second stage of osteochondrosis develops - protrusion.
In the third stage, the fibrous ring breaks down and part of the nucleus pulposus emerges. This is a herniated disc. It puts pressure on the surrounding soft tissues, causes an inflammatory reaction, and so on. Sh.
The fourth stage of osteochondrosis is sequestration of the intervertebral hernia. Part of the pulp nucleus separates or comes out completely with a rupture resulting from a fibrous ring. If the hernia enters the spinal canal cavity, then its delay requires urgent surgical operation. Otherwise, a person may remain paralyzed for the rest of his life with a paralyzed body.
As you can see, this is a very serious disease that needs to be diagnosed in a timely manner. The earlier complex treatment is started, the higher the chance of complete recovery of the intervertebral disc and its functions.
When the first signs of osteochondrosis appear, you can make an appointment with a vertebrologist or neurologist. Doctors will conduct an examination and a manual examination. Make an accurate diagnosis and recommend the necessary additional examinations. After making an accurate diagnosis, you will be offered a course of treatment.
How to diagnose cervical osteochondrosis
How do you know if you have cervical osteochondrosis and not myositis and what to do next? Before diagnosing cervical osteochondrosis, you should collect a medical history:
- When pain appears;
- What actions cause their appearance;
- How long ago was the first convulsion;
- Whether there are any additional clinical signs;
- How the sleeping and workplace are arranged;
- What bad habits there are;
- Workplace and profession.
How do we know that cervical osteochondrosis is based on all this information? First of all, it is important to know that degenerative degenerative disease of the intervertebral discs manifests itself in the form of pain, stiffness of movements, excessive tension of the muscles of the neck and neck area only in the initial stage. Then these signs are added to tension headaches, dizziness, hearing and vision impairment, increased fatigue, impaired mental work and so on. Sh.
A distinctive feature of cervical osteochondrosis is that the aggravation of symptoms begins at the end of the working day. While the patient's professional activity is in most cases associated with prolonged static tension of the muscles of the neck and neck area. On examination, pain is noted on palpation of the vertebral processes of the spine, excessive muscle tension, and an increase in pain when attempting to rotate.
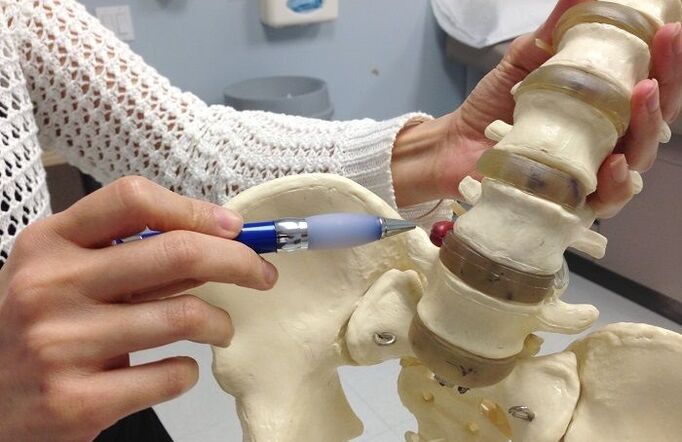
Before diagnosing osteochondrosis of the cervical region, the doctor advises the patient to take an X-ray. It shows reduced spaces between the vertebral bodies. This indicates that protrusion is developing. With the help of X-ray imaging an experienced vertebrologist will be able to rule out the instability of the position of the vertebral bodies, their subluxations, retrolysis, antilhesia, destruction of the intervertebral joints and a number of other serious pathologies. If this examination is not sufficient, then an MRI or CT scan is recommended. If you suspect the development of posterior vertebral artery syndrome, an ultrasound scan of the neck and vessels of the spine is recommended.
How to diagnose osteochondrosis of the chest region
Before diagnosing thoracic osteochondrosis, it is necessary to rule out the possibility of developing pathologies of internal organs such as the heart, coronary circulatory system, lungs, pleura, bronchi, etc. Sh. Consider how to diagnose osteochondrosis of the chest region:
- The most important diagnostic technique is palpation, if the pain is defined only by the vertebral processes of the spine and in the area of the paravertebral muscles, degenerative destruction of the cartilage tissue of the intervertebral discs is not excluded;
- Mobility is limited and any bending and tilting of the body increases the pain;
- The pain attack was provoked by physical exertion, hypothermia, or psychological stress factors;
- Deep breathing does not aggravate the pain.
It is very important to know how to understand heart or osteochondrosis, since acute chest pain is not a rare precursor to myocardial infarction. And in this condition the patient should be urgently provided with cardiac assistance.
So, if you feel anxiety, panic and fear of death during a pain attack, then this is a 90% chance of a heart attack and you should call an ambulance immediately. If there is a tonometer, then you need to measure your blood pressure and calculate your pulse. When the pulse slows down to bradycardia (less than 50 beats per minute) and with an increase in blood pressure to the age norm of 20-40 mm Hg. .
No need to search for information on how to understand heart pain or osteochondrosis, it is much more productive to seek medical help. Even the most common electrocardiogram taken in a hospital emergency department shows what causes the pain syndrome: the heart or spinal column. Independently, you can rely only on sensations on palpation. Typically, with damage to the heart muscle, palpation of the vertebral processes of the spine does not give any unpleasant sensations. But at the same time, there are clinical symptoms of osteochondrosis such as shortness of breath, a feeling of shortness of breath, pale skin, a feeling of cold sticky sweat on the skin, cyanosis of the nasolabial triangle, and severe muscle weakness.
How to diagnose lumbar osteochondrosis
The question of how to understand that lumbar osteochondrosis causes severe pain is quite acute. Moreover, with damage to some paired radicular nerves as well as nerve plexuses, clinical symptoms similar to diseases of the gastrointestinal tract and urinary system appear. These are constipation, diarrhea, frequent urination and so on. Sh.
How to understand that spinal osteochondrosis causes pain and all other clinical signs:
- Does not increase body temperature;
- No nausea and vomiting;
- The tongue is not covered with a white or yellow coating;
- The color of urine when urinating does not differ from normal;
- There are no tenesmus and other sensations of pain when emptying the bowels;
- There is no mixture of blood or mucus in the stool.
A test for Pasternack's symptom is performed to rule out kidney pathology. The patient stands directly with his back to the doctor. The doctor lightly taps the edge of the lower rib arch with the edge of his hand. If pain has occurred, then there is a high probability that lumbar pain is associated with damage to the kidneys and urinary tract.
How to diagnose lumbar osteochondrosis with indirect signs:
- The pain increases dramatically with any movement;
- Aggravation of the condition begins after severe physical exertion, weight lifting, hypothermia or overheating of the body;
- Feel the firmness of movements, often it is associated with muscle weakness;
- The muscles in the lumbar region are sharply tense, painful on palpation;
- The pain may spread along large nerves, for example, in the groin area, on the anterior abdominal wall, along the lower extremities;
- The pain syndrome disappears quickly at rest.
When symptoms characteristic of osteochondrosis appear, it is important to contact a neurologist or vertebrologist as soon as possible. Only an experienced physician can rule out the possibility of spinal dislocation, disc herniation, spinal stenosis and other dangerous pathologies that require urgent medical attention.
What to do about the pain of osteochondrosis
We figured out how to understand that pain arises from osteochondrosis. This is currently important information. You need to know how to behave properly and what you need to do to get rid of such a disease.
Degenerative degenerative disease of the cartilage tissue of the intervertebral discs does not disappear by itself. This is caused by a number of factors. First of all, the surface of the fibrous ring is calcified, as a result of which it loses the ability to absorb the fluid secreted by the working muscles. Second, in the process of reducing the height of the intervertebral discs, secondary compression of the ligaments and tendons occurs. It will be impossible to restore the height of the intervertebral spaces needed to straighten the discs independently.















































