A significant mass of a person falls on his lower back and when lifting a load, twisting from a long static position creates additional stress in him. Excessive load, improper lifestyle continuously leads to degradation of the musculoskeletal system: the spine and the discs between them, which act as a shock absorber. From this point it is worth looking for information about lumbar spine osteochondrosis: symptoms and treatment. Why is the degeneration of the spinal joints?

Degradation of the musculoskeletal system occurs as follows: the natural shock absorber of the spinal column loses elasticity, shrinks, expands the natural boundaries, the pressure on other vertebrae, organs, yoga increases. Let us describe those who are prone to acquire such pathology. Osteochondrosis of the lumbar spine can be observed in humans:
- whose earlier generations suffered from a similar disease;
- having hormonal disorders;
- Individual susceptibility to the development of such diseases (for example, congenital structure of the spine);
- Those who neglect proper nutrition. At the table every day a person should get a balanced diet with healthy fats, vitamins, proteins;
- Those who have a sedentary job: sit or stand in one place for a long time;
- suffers from sharp and heavy loads on the spine, for example: weightlifters, loaders, people working in the garden;
- Diseases of the digestive system, metabolism, pelvic organs;
- Injured (strongly bent on the back, lying on the side, falling, bent);
- reached 30 years of age;
- Diabetes.
If there are signs of lumbar osteochondrosis described in the section below, then some habits should be avoided:
- slash;
- smoking;
- take a bent posture for a long time;
- move slightly;
- Drink alcohol;
- Sit at work without a break;
- Wear not for the weather, let the body cool.
Important. Any disorder in the ligaments is exacerbated by the presence of excess weight. In case of excess weight, the lower body is loaded and the fat-grown waist region is massaged vigorously.
Stages of the disease, its signs
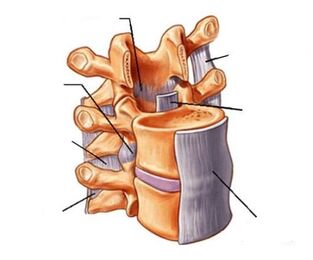
Initially there are periodic mild pains that increase with physical activity. This discomfort indicates that it is time to pay attention to osteochondrosis of the lumbar spine. Currently, the intervertebral discs (the spinal disc is the channel through which the spinal cord and the fibrous ring around it) degrade. Further, the distance between the vertebrae is reduced, the nerves are stretched. The pain intensifies, occupying not only the back but also the thighs and gluteal muscles. In the third stage, the fibrous rings are destroyed, leading to the formation of a spinal hernia, with irreversible deviation, and the pain is constantly there. The fourth stage leads to disability. The special classification of lumbar spine osteochondrosis includes:
- pain;
- ischemic syndrome;
- Radical Syndrome;
- spinal syndrome;
- ossification of adult tissues.
Pain sensations have different degrees of severity and severity: for example, it is called lumbago lumbago; Persistent, aggravated stress, lumbodynia; It is called lumbosalgia along the lower parts of the body. When spinal diseases are not resolved, the spine acquires very free movement in the spinal column. Compression of the nerve roots occurs during weight lifting and sharp actions, then the pain goes from the back but moves to other parts of the body, for which the nerve is responsible. Unconsciously, we change position, adjust so that there is less pain in the back, but it inevitably changes the way the spine walks and bends. It all has to do with a radical syndrome that starts as an irritation and then becomes inflammatory. Signs of lumbar spine osteochondrosis with radicular syndrome:
- Excessive fatigue in the spinal muscles;
- Reverse curve change;
- gait changes;
- swelling of the lower extremities;
- pain in one or both legs;
- severe pain;
- Temporary loss of foot sensitivity;
- periodic prolonged constipation;
- Men have irritability problems;
- Menstrual irregularities in women;
- intoxication of the body;
- blood stagnation.
You may notice that during the break, painful sensations arise and when doing exercises on the back, they cease. Already at this stage you should look for a doctor: chiropractor, surgeon, neurologist, traumatologist (since the causes of osteochondrosis of the lumbar spine include trauma). If the disease progresses, the problem will increase, with the addition of various companions:
- heat;
- numbness;
- sweating;
- tingling;
- chills;
- goose;
- impotence;
- Intestinal colic.
Spinal muscles lose tone and this leads to a general loss of human motor functions. Paralysis is a particularly dangerous course of radical syndrome. Ischemic syndrome is associated with sciatica. At first, the weakening of blood flow is periodic, but then such exhaustion causes spasms. You may notice them while walking normally - you will be in pain if you stop, it will not hurt. Major degradation occurs internally and is not visible to the naked eye - blood flow does not provide the necessary supply to all pelvic organs. There may be pain in the buttocks, thighs and then there may be paralysis of the gluteal muscles. Spinal syndrome involves changes in the skeleton, the blood vessels themselves.
Important. The symptoms of lumbar osteochondrosis in women are inextricably linked to the hormonal background, the physiological characteristics of the body. Occurrence of pain, improper posture affects the wearing of unsuitable shoes: too hard or too soft soles; Too high heel or too low heel.
Diagnosis of disease stages

It can be very difficult for a doctor to classify and name the stage of a disease during a disease examination. Initially, a neurologist can diagnose:
- permanent curvature of the spinal column;
- pain on touch;
- decreased leg movement;
- gluteal zone asymmetry;
- Replace the Michaelis diamond.
But the most accurate diagnosis can only be made with the results:
- Computed tomography (CT). The most optimal option for determining the degree of disease development, which allows to assess the stage of degeneration of the spinal column.
- X-ray. In their view, it is possible to determine the presence of disease, but it is not always possible to determine the degree of development of damage to nerve fibers and blood vessels.
- Magnetic resonance imaging. Quite a long (from half an hour to an hour), expensive procedure that additionally offers the most complete details about what happens to the nerve roots and blood vessels.
Thus, the physician can finally assess osteochondrosis of the lumbar spine: symptoms and treatment based solely on the results of the device examination. Lumbar pain that is not associated with a lumbar disc herniation is caused by a cold, kidney cold, menstrual cycle, or back pain.
Important. CT, X-ray examinations are not acceptable for pregnant women. CT is not safe: 1) for children under 14 years; 2) People with iodine allergy.
Medical treatment
The reasons for the onset of the disease, its characteristics have been discussed above, now let’s move on to the second point of lumbar spine osteochondrosis: symptoms and treatment. The longer you ignore the body's signals, the faster the disease will develop. The earlier you start, the more medication and procedure you need to use. Treatment goals:
- Identify, eliminate the causes of root, spinal blood vessels;
- restores skin sensitivity;
- to prevent further development of pathology;
- Start body processes for self-healing;
- Enhance human muscle tone;
- Restoring the function of the internal organs of the small pelvis;
- Return to normal lumbar spine flow.
If you experience any discomfort, consult your doctor. The first thing to do at the first symptoms is to pay attention to: the bed (a wide selection of orthopedic mattresses that should be selected individually), the pillow (may not fit in size or tenderness), the position during sleep, the movement. At home, without examination by a doctor, lumbar spine osteochondrosis is treated only by bed rest. Therefore, a visit to the doctor is mandatory. Various medications are taken during the remission phase and the acute phase of the disease. In the last phase, medications are used to relieve pain, free the nerves from spinal mites, and eliminate inflammation. Schedule: - blockade; - Glucocorticoids; - Chondroprotectors; - Myo-laxatives; - Nonsteroidal anti-inflammatory drugs (NSAIDs).

The last group of drugs, in addition to relieving pain, fights excessive body temperature, edema, inflammation. Such funds may be: rectum, for internal use, injection, external. Treatment of lumbar spine osteochondrosis most often begins with nonsteroidal anti-inflammatory drugs:
- diclofenac;
- piroxicam;
- ibuprofen;
- Himeculide;
- Hapox;
- dexketoprofen;
- meloxicam;
- aceclofenac.
Anti-inflammatory drugs in this list are various ointments, tablets, gels. Some tabular anti-inflammatory drugs have contraindications for ulcers or gastritis. Muscle relaxants relieve joint density and involuntary contraction of the back muscles by temporarily reducing muscle tone. This group of drugs includes tizanidine, tolperisone hydrochloride. Chondroprotectors are prescribed when there is a possibility of survival of the intervertebral disc, which should serve to restore anal fibrosis. The course of taking such a group of drugs is very long - at least 1, 5 months and the results can be seen only after a year. They try to avoid prescribing glucocorticoids as they have side effects due to their intake as the drugs in this group belong to the steroid hormones. They should be taken under the supervision of the attending physician, following all prescriptions, since only a specialist knows how to cure lumbar osteochondrosis. An example of such a drug is hydrocortisone. Blocking is not a medication in itself, but they are a strong local pain reliever. The technique is as follows: Injecting pain relief (IO) or a combination of IO from the glucocorticoid group into the pain area. Blockades do not have healing properties, but they can be addictive, leading to a loss of sensitivity to these drugs. If injected frequently, the muscles around the injection may atrophy. Therefore, when acute pain is reduced by this method, the patient is prescribed medications aimed at restoring damaged tissues, blood flow, and improving muscle and nerve fiber tone. this:
- Chondroprotectors, which have a general enhancing effect on bone tissue, normalize cartilage tissue metabolism.
- Vitamins that help restore nerve conduction.
- Biogenic drugs that help the body heal itself;
- Vascular drugs that thin the blood to improve the nutrition of internal organs.
During treatment, antidepressants are prescribed in addition to the main medication. Here's how to treat low back osteochondrosis to reduce acute pain:
- Use warming, analgesic, anti-inflammatory external remedies;
- Do special exercises for the back;
- go for a massage;
- Live a gentle lifestyle;
- Wear a belt corset while exercising.
Massage, exercise therapy, physiotherapy and alternative therapies.

Relatively inexpensive, effective methods of combating the degradation of shock absorbers are physiotherapy exercises, massage, physiotherapy. Only a professional with a medical education can do a real massage, so a simple visit to a beauty salon is not suitable for patients. Each stage of the disease requires different pressures and techniques. With proper therapy, the muscle spasm disappears, the spinal muscular framework strengthens, and the pain gradually disappears. Physiotherapy is used only in the process of weakening painful processes or in their absence (to maintain the movement of the spine). Gymnastics is selected individually, according to age, mouth condition, stage of disease development. The productivity of therapeutic exercises directly depends on the quality and frequency of performance: they must be done systematically. It is recommended to rest at home, lie on your back, bend your legs, place a small roller under the lower roller. The healing process is monitored with the help of X-rays, tomographic surveys. Physiotherapeutic treatment is prescribed during remission and exacerbation. Methods such as:
- Acupuncture. The oldest method of pain treatment based on stimulating acupuncture points with thin needles. The procedure relieves spasms, reduces pain, completely eliminates it, reduces tissue swelling;
- Ultraviolet radiation that stimulates the body to absorb calcium;
- ampilpus, named from the corresponding device. The treatment procedure is as follows: the plates of the apparatus are fixed at the back, and the corresponding therapeutic current flows in the plates with different parameters;
- Laser therapy. Laser rays relieve pain, heal, stop inflammation in the lumbar region;
- Darsonvalization. The method aims to improve blood circulation, dilate blood vessels, stimulate nerve endings;
- Phonophoresis is treated with ultrasound, stimulating blood circulation in the muscular part of the dorsal region.
Each method has its own contraindications. Traditional medicine is more complicated. Official medicine does not recognize that midwives know how to treat lumbar osteochondrosis. Therefore, if a friend advises you to use compresses made of barberry broth, take pine baths, you should consult a doctor. A method such as hirudotherapy is used for anesthesia, but the secrets behind this name are hidden, so doctors recommend that you approach this method of treatment with caution.
Solve a Surgical Problem
In some cases it is impossible to do without surgery. With advanced interstitial hernia, neurosurgeons use microdiscectomy. The operation removes the damaged disc. If there are no contraindications, then doctors can do nucleoplasty, which has many advantages:
- does not require wounds;
- operation lasts up to 30 minutes;
- No restrictions on surgical procedures.
Important. To maintain the mobility of the spine, strengthen the spinal muscles, it is recommended to do yoga, swimming, Pilates. Jogging creates a shock load on the back of the spine, so you should stop jogging at the first sign of low back pain.















































